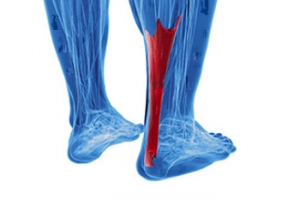
Achilles Tendon Bursitis
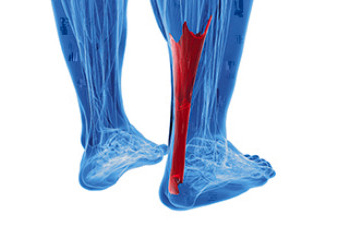
Achilles tendon bursitis is a painful condition that involves inflammation of the fluid filled sac, or bursa, located between the skin of the heel. Posterior Achilles tendon bursitis affects the back of the heel, while anterior Achilles tendon bursitis, also called retromalleolar bursitis, is felt in front of the attachment of the Achilles tendon to the heel bone. Symptoms include swelling, warmth, pain, and a tender spot at the back of the heel. Diagnosis by a podiatrist begins with a discussion of symptoms and a medical history, followed by a physical examination to identify signs of inflammation and tenderness. X-rays may be used to rule out other potential causes of heel pain, and in some cases, an ultrasound or MRI may provide more detailed views. The primary goal is to relieve inflammation and reduce pain. Treatment approaches may vary based on the severity and location of the pain. In rare cases, surgical intervention may be considered. For help in relieving the pain of Achilles tendon bursitis, it is suggested that you make an appointment with a podiatrist.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
Achilles Tendon Injuries
The Achilles tendon is the largest tendon in the body; it is a tough band of fibrous tissue that stretches from the bones of the heel to the calf muscles. This tendon is what allows us to stand on our toes while running, walking, or jumping, it is common for this tendon to become injured. In severe cases, the Achilles tendon may become partially torn or completely ruptured. However, this tendon is susceptible to injury because of its limited blood supply and the high level of tension it endures.
The people who are more likely to suffer from Achilles tendon injuries are athletes who partake in activities that require them to speed up, slow down, or pivot. Consequently, athletes who engage in running, gymnastics, dance, football, baseball, basketball, or tennis are more likely to suffer from Achilles tendon injuries. Additionally, there are other factors that may make you more prone to this injury. People who wear high heels, have flat feet, tight leg muscles or tendons, or take medicines called glucocorticoids are more likely to have Achilles tendon injuries.
A common symptom of an Achilles tendon injury is pain above the heel that is felt when you stand on your toes. However, if the tendon is ruptured, the pain will be severe, and the area may become swollen and stiff. Other symptoms may be reduced strength in the lower ankle or leg area, and reduced range of motion in the ankle. When the Achilles tendon tears, there is usually a popping sound that occurs along with it. People who have acute tears or ruptures may find walking and standing to be difficult.
If you suspect you have injured your Achilles tendon, you should see your podiatrist to have a physical examination. Your podiatrist will likely conduct a series of tests to diagnose your injury including a “calf-squeeze” test. Calf squeeze tests are performed by first squeezing the calf muscle on the healthy leg. This will pull on the tendon and consequently cause the foot to move. Afterward, the same test will be performed on the injured leg. If the tendon is torn, the foot won’t move because the calf muscle won’t be connected to the foot.
Types of Flat Feet

Flatfoot is characterized by the loss of the foot's arch, leading to an abducted forefoot and a hindfoot deformity. The two types of flat feet are flexible and rigid flatfoot. In flexible flatfoot, the arch appears when not bearing weight, but disappears when weight is applied. Conversely, in rigid flatfoot, the arch is consistently absent. Flexible flatfoot often appears in young children and may self-resolve. Its frequency in adults is unclear, due to frequent misdiagnosis. The disorder can be either congenital or developed over time. Flexible flatfoot results from ligament laxity, while adult-acquired flatfoot is attributed to posterior tibial tendon insufficiency, potentially caused by factors like obesity, neuropathy, or trauma. Rigid flatfoot results from bone irregularities or arthritis. A missing foot arch and deformities are noticeable upon examination. If you have flatfoot and it is causing you discomfort, it is suggested that you make an appointment with a podiatrist who can determine which type of flat foot you have, in addition to providing appropriate relief and treatment options.
Flatfoot is a condition many people suffer from. If you have flat feet, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors will treat your foot and ankle needs.
What Are Flat Feet?
Flatfoot is a condition in which the arch of the foot is depressed and the sole of the foot is almost completely in contact with the ground. About 20-30% of the population generally has flat feet because their arches never formed during growth.
Conditions & Problems:
Having flat feet makes it difficult to run or walk because of the stress placed on the ankles.
Alignment – The general alignment of your legs can be disrupted, because the ankles move inward which can cause major discomfort.
Knees – If you have complications with your knees, flat feet can be a contributor to arthritis in that area.
Symptoms
- Pain around the heel or arch area
- Trouble standing on the tip toe
- Swelling around the inside of the ankle
- Flat look to one or both feet
- Having your shoes feel uneven when worn
Treatment
If you are experiencing pain and stress on the foot you may weaken the posterior tibial tendon, which runs around the inside of the ankle.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Flat Feet
Flatfoot is a foot condition in which the arch of the foot has either partially or totally dropped or has never developed. While it is common in babies and small children, it can become a problem for them in adulthood if the arch never forms. For adults, the development of flat feet can be brought upon by injury, as a result of pregnancy due to increased elasticity, or obesity. Those who have health concerns such as rheumatoid arthritis or diabetes may also be at greater risk for developing the condition.
If you suspect that you have flat feet, it is best to consult your podiatrist. Your foot doctor will examine the suspected foot and observe how it looks while you sit and stand. He or she may take an X-ray to determine how serious the condition is. Some common signs of flatfoot include toe drift, in which the toes and front part of the foot point outward, a short Achilles tendon, and a heel that tilts outwardly while the ankle tilts inward.
Once flatfoot has been diagnosed, your podiatrist may suggest one of several treatment options. Flat feet can be rigid, in which the feet appear to have no arch even when the person is not standing; or flexible, in which the person appears to have an arch while not standing, but once standing the arch disappears. Those with flexible flatfoot may be told to reduce any activities that cause pain and to avoid extended periods of walking or standing. Another suggestion may be weight loss, as excessive weight may be placing pressure on the arches
In few cases, if the condition is severe and all other methods have been exhausted surgery may be required. This is normally avoided, however, due to a lengthy recovery time and high cost.
Foot Blisters Are a Common Foot Ailment

Foot blisters are pockets of fluid that form on the skin's surface, and can turn a pleasant walk or workout into a painful experience. These common nuisances are often the result of friction or repeated rubbing on the skin. When the skin experiences excessive pressure or friction, the top layer separates from the layers beneath, trapping a small amount of fluid in the newly formed pocket. Blisters can also be caused by wearing ill-fitting shoes, footwear that rubs against the skin, high levels of moisture, or extended periods of physical activity. Understanding the factors that contribute to blister formation is essential for prevention. If you have developed a blister on your foot that has become problematic, it is suggested that you speak with a podiatrist who can properly treat it and offer you effective prevention methods.
Blisters may appear as a single bubble or in a cluster. They can cause a lot of pain and may be filled with pus, blood, or watery serum. If your feet are hurting, contact one of our podiatrists of Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Foot Blisters
Foot blisters are often the result of friction. This happens due to the constant rubbing from shoes, which can lead to pain.
What Are Foot Blisters?
A foot blister is a small fluid-filled pocket that forms on the upper-most layer of the skin. Blisters are filled with clear fluid and can lead to blood drainage or pus if the area becomes infected.
Symptoms
(Blister symptoms may vary depending on what is causing them)
- Bubble of skin filled with fluid
- Redness
- Moderate to severe pain
- Itching
Prevention & Treatment
In order to prevent blisters, you should be sure to wear comfortable shoes with socks that cushion your feet and absorb sweat. Breaking a blister open may increase your chances of developing an infection. However, if your blister breaks, you should wash the area with soap and water immediately and then apply a bandage to the affected area. If your blisters cause severe pain it is important that you call your podiatrist right away.
If you have any questions, please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Blisters
Blisters are pockets of fluid that occur under the top layer of your skin. These fluid pockets are usually filled with pus, blood, or serum. Blisters may itch or hurt and can appear as a single bubble or in clusters.
The most common types of blisters are friction blisters. This type of blister may be caused by wearing shoes that are too tight. Friction blisters can also occur on the hands. A change in temperature may also cause blisters on the feet. In the freezing air, frostbite on your toes can lead to blisters, as well as sunburn from hot weather.
The best way to treat a blister is to keep it clean and dry. Most blisters will get better on their own. Once the skin absorbs the fluid within the blister, it will flatten and eventually peel off. You should avoid popping your blister unless you podiatrist does it for you. Additional treatment options include applying an ice pack to the blister or using over-the-counter blister bandages to cover the affected area.
If your blister becomes discolored, inflamed, or worsens it is advised that you speak to your podiatrist. Blisters that are yellow, green, or purple may be infected and require immediate medical attention. Blisters that are abnormally colored may be a sign of a more serious underlying health condition such as herpes.
Aftercare for a Foot Fracture

A foot fracture can be a painful and distressing experience, disrupting daily life and mobility. However, the journey to recovery does not end with the diagnosis and proper aftercare is paramount. Immobilization, typically through a cast, splint, or walking boot, is essential to stabilize the foot and promote healing. Elevating the foot can help to reduce swelling and promote circulation. Pain management, as prescribed by a healthcare professional, ensures comfort during the healing process. Getting adequate rest is essential, and avoiding putting weight on the injured foot is advised. As healing progresses, gentle exercises can aid in regaining strength and mobility. Following your podiatrist's recommendations and attending follow-up appointments are vital for a smooth recovery. Patience, care, and adherence to the prescribed aftercare regimen are key to returning to normal activities with a healed foot. If you have broken your foot, it is strongly suggested that you consult a podiatrist who can guide you toward the correct recovery plan that is right for you.
A broken foot requires immediate medical attention and treatment. If you need your feet checked, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Broken Foot Causes, Symptoms, and Treatment
A broken foot is caused by one of the bones in the foot typically breaking when bended, crushed, or stretched beyond its natural capabilities. Usually the location of the fracture indicates how the break occurred, whether it was through an object, fall, or any other type of injury.
Common Symptoms of Broken Feet:
- Bruising
- Pain
- Redness
- Swelling
- Blue in color
- Numbness
- Cold
- Misshapen
- Cuts
- Deformities
Those that suspect they have a broken foot shoot seek urgent medical attention where a medical professional could diagnose the severity.
Treatment for broken bones varies depending on the cause, severity and location. Some will require the use of splints, casts or crutches while others could even involve surgery to repair the broken bones. Personal care includes the use of ice and keeping the foot stabilized and elevated.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Causes, Symptoms, and Treatment for a Broken Foot
The human foot has 26 different bones, and the foot is divided into three parts: the hindfoot, the midfoot, and the forefoot. Each section of the foot is composed of a different amount of bones. For instance, the forefoot is made up of 19 bones. The midfoot is composed of five smaller bones called the navicular, cuboid, and three cuneiform bones. Lastly, the hindfoot is made up of only the talus and the calcaneus. The feet tend to be vulnerable to slipping and twisting; consequently, fractured bones within the foot are common. When a bone gets crushed, bent, twisted, or stretched it may become broken.
Many foot fractures occur through an accident or trauma. More specifically, common causes for broken feet are car accidents, falls, missteps, or overuse. If you have a broken ankle or foot, you may have one or more of the following symptoms: throbbing pain, swelling, bruising, tenderness, deformities, and difficulty walking.
There are some factors that may put you at a higher risk of developing a broken foot. People who participate in high-impact sports are more likely to develop foot fractures because of the stresses, direct blows, and twisting injuries involved in gameplay. Additionally, those who suddenly increase their activity level are more likely to suffer a stress fracture.
Unfortunately, there are different complications that may arise because of a foot fracture. For instance, arthritis may be caused by fractures that extend into the joints. Bone infections are also possible in open fractures due to the bone being exposed to bacteria. However, there are ways you can help prevent yourself from breaking your foot. One way to avoid fractures is to wear proper footwear. If you plan on going on a run, you should wear running shoes. You should also replace your shoes if you notice that they are becoming worn out. For runners, it is best to replace shoes every 300 to 400 miles.
Treatment for foot fractures usually consists of rest, ice, elevation, and compression (RICE). If you plan on wrapping your foot, try not to wrap it too tightly because doing so may cut off blood supply in the foot. You should also avoid walking on the fractured foot.
If you suspect you have a broken foot, you should see your podiatrist right away. It is important that you have someone bring you to your doctor, since driving with a broken foot can be dangerous. You should especially seek urgent care if you are experiencing numbness, pain, or deformities in your foot.
Common Causes of Foot Pain in Seniors

Foot pain is a common complaint among seniors, affecting approximately 20 percent of older adults regularly. Among the most common causes of foot pain in seniors are stress fractures, heel pain, diabetic neuropathy, gout, and blood clots. Seniors are more susceptible to stress fractures due to age-related changes in bone density. Stress fractures are tiny cracks in bones that typically manifest as pain during activity, but subside with rest. Plantar fasciitis, characterized by irritation and inflammation of the plantar fascia ligament on the sole of the foot, can cause persistent heel pain. Diabetes frequently leads to neuropathy, which causes tingling, burning, or numbness in the feet. Regular foot monitoring and care are essential for individuals with diabetes to prevent complications. A podiatrist can help manage conditions such as corns, calluses, and nail care. Gout, a form of inflammatory arthritis, typically affects the big toe. Sudden and severe pain, especially at night, may indicate gout. Blood tests or joint fluid analysis can confirm the diagnosis. Deep vein thrombosis, or a blood clot, is often associated with leg swelling and pain, but it can also cause sudden and severe pain in the ankle or foot. Seniors, especially those who smoke, are overweight, or are sedentary, may be at a higher risk. If you are experiencing foot or ankle pain that persists or worsens, it is suggested that you make an appointment with a podiatrist for treatment options.
Proper foot care is something many older adults forget to consider. If you have any concerns about your feet and ankles, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
The Elderly and Their Feet
As we age we start to notice many changes in our body, but the elder population may not notice them right away. Medical conditions may prevent the elderly to take notice of their foot health right away. Poor vision is a lead contributor to not taking action for the elderly.
Common Conditions
- Neuropathy – can reduce feeling in the feet and can hide many life-threatening medical conditions.
- Reduced flexibility – prevents the ability of proper toenail trimming, and foot cleaning. If left untreated, it may lead to further medical issues.
- Foot sores – amongst the older population can be serious before they are discovered. Some of the problematic conditions they may face are:
- Gouging toenails affecting nearby toe
- Shoes that don’t fit properly
- Pressure sores
- Loss of circulation in legs & feet
- Edema & swelling of feet and ankles
Susceptible Infections
Diabetes and poor circulation can cause general loss of sensitivity over the years, turning a simple cut into a serious issue.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.