Vascular Testing in Podiatry
In foot care, vascular testing may be required in the diagnosing and treatment of certain podiatric conditions. Vascular testing is particularly relevant for patients with high-risk diabetes, poor circulation, peripheral artery disease (PAD), and chronic venous insufficiency (CVI). Procedures typically involve the examination of blood vessels throughout the body for blockages or buildup.
Vascular testing is very important for the diagnosis of various conditions, including peripheral artery disease and chronic venous insufficiency, as these conditions can greatly affect one’s quality of life and cause pain in the lower limbs. Circulatory problems in the feet and ankles can reflect issues throughout the body, making testing of the blood vessels pertinent.
Testing methods vary between practitioners and can be specific to certain foot and ankle problems. Modern technology has brought about the ability to perform vascular testing using non-invasive methods, such as the cuff-based PADnet testing device. This device records the Ankle-Brachial Index (ABI)/Toe-Brachial Index (TBI) values and Pulse Volume Recording (PVR) waveforms. Contact your podiatrist to determine what vascular testing is available for your needs.
Dealing With a Dislocated Toe

The most common cause of a dislocated toe is direct injury, either bumping into something solid or dropping something heavy on it. You most likely will feel extreme pain at the time of the injury, it will be hard to bend, or even move the toe; and it will swell, become bruised or lose feeling. Sometimes a loose ligament will cause a toe to dislocate, which is extremely painful. Avoid trying to pop the toe into place yourself, as this may cause further injury. The first thing to do is stop further activity, elevate the foot, immobilize it, and apply ice. Next, make an appointment with a podiatrist immediately. An X-ray may be required, followed by manipulating the bones back into place. Followup treatments include strapping the injured toe to the one next to it, alternating ice and heat, undergoing whirlpool treatments, and doing strengthening exercises. A podiatrist can properly diagnose the severity of your toe injury and propose the proper treatment plan for you.
A broken toe can be very painful and lead to complications if not properly fixed. If you have any concerns about your feet, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors will treat your foot and ankle needs.
What to Know About a Broken Toe
Although most people try to avoid foot trauma such as banging, stubbing, or dropping heavy objects on their feet, the unfortunate fact is that it is a common occurrence. Given the fact that toes are positioned in front of the feet, they typically sustain the brunt of such trauma. When trauma occurs to a toe, the result can be a painful break (fracture).
Symptoms of a Broken Toe
- Throbbing pain
- Swelling
- Bruising on the skin and toenail
- The inability to move the toe
- Toe appears crooked or disfigured
- Tingling or numbness in the toe
Generally, it is best to stay off of the injured toe with the affected foot elevated.
Severe toe fractures may be treated with a splint, cast, and in some cases, minor surgery. Due to its position and the pressure it endures with daily activity, future complications can occur if the big toe is not properly treated.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
What to Know About a Broken Toe
The forefoot is composed of five metatarsal bones and fourteen phalanges. Each toe has three phalanges except for the big toe which only has two. Our toes play an essential role to the walking process, which is why a broken toe could seriously disrupt one’s ability to move around. Toe fractures are common and can be very painful. Fortunately, these injuries rarely require surgery and usually heal with rest and a change in activity.
Broken toes typically result from a traumatic event such as falling, stubbing the toe, or dropping something on the toe. Traumatic toe fractures may be categorized as either minor or severe fractures. At times, one may hear a “pop” or “crack” sound when the bone breaks. Common symptoms of a traumatic toe fracture include pain, throbbing, bruising, swelling, and redness.
Another type of toe fractures is a stress fracture. These injuries usually appear in the form of small hairline breaks on the bone. Stress fractures develop after repetitive activity instead of a single injury. Stress fractures occur when the muscles in the bone become too weak to absorb impact. Consequently, the toe bone becomes vulnerable to any pressure and impact it endures. Symptoms for a stress fracture in the toe include swelling without bruising, tenderness to the touch, pain that goes away with rest, and pain after walking or running.
If you suspect that you have a broken toe, you should make an appointment with your podiatrist. He or she will likely diagnose you by performing a physical exam and an X-ray. Treatment for a broken toe may include the R.I.C.E. method, buddy taping, surgery, or antibiotics. The R.I.C.E. method (Rest, Ice, Compression, and Elevation) is a common treatment method for many injuries because it decreases pain. Buddy tapping involves wrapping the injured toe next to an adjacent toe to keep it supported and protected. These two methods have proven to be effective in the healing process for toe fractures. The estimated healing time for a broken toe is approximately four to six weeks. If the injury becomes infected or requires surgery, the estimated healing time may take eight weeks or more.
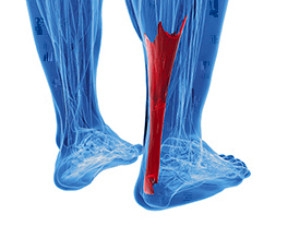
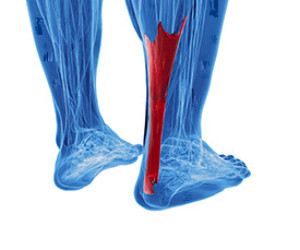
Risks of an Achilles Rupture
When you experience a complete tear of the Achilles tendon in the ankle, it is called an Achilles rupture. The list of those most likely to have this condition can include: men over 40, athletes who play sports such as football, tennis, or rugby, women who wear high heels, athletes who consistently ignore Achilles pain, and athletes who have had a recent ankle injury, overpronate, or have a thinner Achilles tendon. Still other risk factors include being overweight, taking certain medications, or using corticosteroids. What does a ruptured Achilles tendon feel like? It reportedly feels like someone has kicked or hit you in the back of the heel. Ignoring the warning signs, such as a pain that builds gradually or the pain from another ankle injury, increases the risk of such a tear. To avoid this occurrence, it is a good idea to see a podiatrist, who can perform a full biomechanical analysis to determine whether you may need orthotics or specific stretching and strengthening exercises. It is possible to recover from this painful event, but prevention is better.
Achilles tendon injuries need immediate attention to avoid future complications. If you have any concerns, contact one of our podiatrists of Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is the Achilles Tendon?
The Achilles tendon is a tendon that connects the lower leg muscles and calf to the heel of the foot. It is the strongest tendon in the human body and is essential for making movement possible. Because this tendon is such an integral part of the body, any injuries to it can create immense difficulties and should immediately be presented to a doctor.
What Are the Symptoms of an Achilles Tendon Injury?
There are various types of injuries that can affect the Achilles tendon. The two most common injuries are Achilles tendinitis and ruptures of the tendon.
Achilles Tendinitis Symptoms
- Inflammation
- Dull to severe pain
- Increased blood flow to the tendon
- Thickening of the tendon
Rupture Symptoms
- Extreme pain and swelling in the foot
- Total immobility
Treatment and Prevention
Achilles tendon injuries are diagnosed by a thorough physical evaluation, which can include an MRI. Treatment involves rest, physical therapy, and in some cases, surgery. However, various preventative measures can be taken to avoid these injuries, such as:
- Thorough stretching of the tendon before and after exercise
- Strengthening exercises like calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
What are Achilles Tendon Injuries
The Achilles tendon is the strongest tendon in the human body. Its purpose is to connect the lower leg muscles and calf to the heel of the foot. This tendon is responsible for facilitating all types of movement, like walking and running. This tendon provides an enormous amount of mobility for the body. Any injuries inflicted to this tissue should be immediately brought up with a physician to prevent further damage.
The most common injuries that can trouble the Achilles tendon are tendon ruptures and Achilles tendinitis. Achilles tendinitis is the milder of the two injuries. It can be recognized by the following symptoms: inflammation, dull-to-severe pain, increased blood flow to the tendon, thickening of the tendon, and slower movement time. Tendinitis can be treated via several methods and is often diagnosed by an MRI.
An Achilles tendon rupture is trickier to heal, and is by far the most painful injury. It is caused by the tendon ripping or completely snapping. The results are immediate and absolutely devastating, and will render the patient immobile. If a rupture or tear occurs, operative and non-operative methods are available. Once the treatment begins, depending on the severity of the injury, recovery time for these types of issues can take up to a year.
Simple preventative measures can be taken as a means to avoid both injuries. Prior to any movement, taking a few minutes to stretch out the tendon is a great way to stimulate the tissue. Calf raises, squats, leg curls, leg extensions, leg raises, lunges, and leg presses are all suggested ways to help strengthen the lower legs and promote Achilles tendon health.
Many problems arise among athletes and people who overexert themselves while exercising. Problems can also happen among those who do not warm up properly before beginning an activity. Proper, comfortable shoes that fit correctly can also decrease tendon injuries. Some professionals also suggest that when exercising, you should make sure that the floor you are on is cushioned or has a mat. This will relieve pressure on the heels. A healthy diet will also increase tendon health.
It is very important to seek out a podiatrist if you believe you have an injury in the Achilles region. Further damage could result in severe complications that would make being mobile difficult, if not impossible.
Symptoms May be Gradual With a Stress Fracture
 Excess pressure that is exerted on a bone in the foot can lead to a stress fracture. It can develop from practicing high-impact exercise, increasing speed and training too fast, or possible from poor nutrition. This type of injury develops slowly, and symptoms are often ignored. It can become difficult to complete daily activities, and it helps to temporarily stop the activity that caused the injury. After a proper diagnosis is made, which generally occurs when an X-ray is taken, treatment can begin. A walking boot or a cast may be helpful in stabilizing the foot as the healing process takes place. The average time for a stress fracture to heal is four to six weeks, and then a gradual return to the chosen activity is often advised. If you have a stress fracture, please consult with a podiatrist as quickly as possible who can help you with the correct treatment plan.
Excess pressure that is exerted on a bone in the foot can lead to a stress fracture. It can develop from practicing high-impact exercise, increasing speed and training too fast, or possible from poor nutrition. This type of injury develops slowly, and symptoms are often ignored. It can become difficult to complete daily activities, and it helps to temporarily stop the activity that caused the injury. After a proper diagnosis is made, which generally occurs when an X-ray is taken, treatment can begin. A walking boot or a cast may be helpful in stabilizing the foot as the healing process takes place. The average time for a stress fracture to heal is four to six weeks, and then a gradual return to the chosen activity is often advised. If you have a stress fracture, please consult with a podiatrist as quickly as possible who can help you with the correct treatment plan.
Activities where too much pressure is put on the feet can cause stress fractures. To learn more, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep your pain free and on your feet.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures occur in the foot and ankle when muscles in these areas weaken from too much or too little use. The feet and ankles then lose support when walking or running from the impact of the ground. Since there is no protection, the bones receive the full impact of each step. Stress on the feet can cause cracks to form in the bones, thus creating stress fractures.
What Are Stress Fractures?
Stress fractures occur frequently in individuals whose daily activities cause great impact on the feet and ankles. Stress factors are most common among:
- Runners
- People affected with Osteoporosis
- Tennis or basketball players
- Gymnasts
- High impact workouts
Symptoms
Pain from the fractures occur in the area of the fractures and can be constant or intermittent. It will often cause sharp or dull pain with swelling and tenderness. Engaging in any kind of activity which involves high impact will aggravate pain.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Dealing with Stress Fractures of the Foot and Ankle
Stress fractures are small breaks in the bone that are caused by repetitive stress. They typically occur due to overuse, forcing the bones of the foot or ankle to continually absorb the full impact of each step taken. Stress fractures can also be caused by abnormal foot structure, osteoporosis, bone deformities, or wearing improper footwear during exercise.
Stress fractures are common for individuals whose daily activities cause high levels of impact on their feet and ankles. Those who run, play tennis or basketball, or practice gymnastics tend to experience these fractures more frequently. Anyone is susceptible to this problem, though. Individuals who are normally sedentary and suddenly begin an intense, high impact workout may sustain stress fractures. This is because their muscles are not yet strong enough to handle and cushion the intensity of their activity. Osteoporosis may also cause someone to get stress fractures, because the disease weakens an afflicted person's bones and makes it easier for them to break down.
Pain from stress fractures typically occurs in the general area of the fracture. Pain can also manifest as “pinpoint pain” or pain that is felt when the site of the injury is touched, and can be accompanied by swelling. It may occur during or after activity, and it may disappear while resting and return when standing or moving. Engaging in any kind of activity, high impact or otherwise, will aggravate the pain. If the intensity of the activity increases before the stress fracture has properly healed, it can cause a full fracture.
Treatment can vary depending on the individual and the degree of injury. The primary way to treat a stress fracture is to rest the hurt foot. Some fractures will heal quickly with only a little bit of rest, while others may require a long rest period and the use of crutches, immobilization, or physical therapy. Under certain circumstances, surgery may be required to install support pins around the fracture to assist in healing.
If you are undergoing a new exercise regimen in running or some other kind of high impact activity, set incremental goals on a weekly basis so you can build up muscle strength. Make sure to wear supportive shoes to better protect you feet.
If you begin to experience any symptoms of stress fractures, you should stop exercising and rest. If the symptoms persist, consult with your podiatrist. Remembering these tips can help you prevent stress fractures to your foot and ankle, and allow you to continue living normally.
The Danger of Wounds in People With Diabetes
Wounds are a major concern for people with diabetes. Prolonged elevated blood sugar levels can lead to nerve damage and poor circulation. Both conditions can make it very difficult for the diabetic to detect, and for their body to heal, developing wounds on their feet. Wounds that do not heal can lead to much more dangerous conditions such as ulcers, infections, gangrene, and in severe cases, amputation. To avoid these worst-case scenarios, diabetics should avoid wounds from developing in the first place. Wearing comfortable shoes that fit well and do not rub against the skin is one way to prevent blisters, corns, calluses, or other problematic issues from developing. To minimize the risks of cuts or scrapes, walking barefoot should be avoided. The feet should be inspected daily for any cuts, abrasions, red spots, blisters, or anything unusual. Any irregularity should be immediately reported to a podiatrist. Finally, regular checkups with a podiatrist are critical for every diabetic to keep wounds at bay and to receive prompt and professional treatment should a wound develop.
Diabetic foot care is important in preventing foot ailments such as ulcers. If you are suffering from diabetes or have any other concerns about your feet, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Diabetic Foot Care
Diabetes affects millions of people every year. The condition can damage blood vessels in many parts of the body, especially the feet. Because of this, taking care of your feet is essential if you have diabetes, and having a podiatrist help monitor your foot health is highly recommended.
The Importance of Caring for Your Feet
- Routinely inspect your feet for bruises or sores.
- Wear socks that fit your feet comfortably.
- Wear comfortable shoes that provide adequate support.
Patients with diabetes should have their doctor monitor their blood levels, as blood sugar levels play such a huge role in diabetic care. Monitoring these levels on a regular basis is highly advised.
It is always best to inform your healthcare professional of any concerns you may have regarding your feet, especially for diabetic patients. Early treatment and routine foot examinations are keys to maintaining proper health, especially because severe complications can arise if proper treatment is not applied.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Diabetic Foot Care
Diabetes can cause two problems that can potentially affect the feet: Diabetic neuropathy and Peripheral Vascular Disease. Diabetic neuropathy occurs when nerves in your legs and feet become damaged, which prevents you from feeling heat, cold, or pain. The problem with diabetic neuropathy is that a cut or sore on the foot may go unnoticed and the cut may eventually become infected. This condition is also a main cause of foot ulcers. Additionally, Peripheral vascular disease also affects blood flow in the body. Poor blood flow will cause sores and cuts to take longer to heal. Infections that don’t heal do to poor blood flow can potentially cause ulcers or gangrene.
There are certain foot problems that are more commonly found in people with diabetes such as Athlete’s foot, calluses, corns, blisters, bunions, foot ulcers, ingrown toenails, and plantar warts. These conditions can lead to infection and serious complications such as amputation. Fortunately, proper foot care can help prevent these foot problems before they progress into more serious complications.
Each day you should wash your feet in warm water with a mild soap. When you finish washing your feet, dry them carefully especially between your toes. You should also perform daily foot inspections to ensure you don’t have any redness, blisters, or calluses. Furthermore, if you are diabetic, you should always wear closed-toed shoes or slippers to protect your feet. Practicing these tips will help ensure that your feet are kept healthy and away from infection.
If you have diabetes, contact your podiatrist if you have any of the following symptoms on your feet: changes in skin color, corns or calluses, open sores that are slow to heal, unusual and persistent odor, or changes in skin temperature. Your podiatrist will do a thorough examination of your feet to help treat these problematic conditions.