Seeing a Podiatrist for Plantar Fasciitis
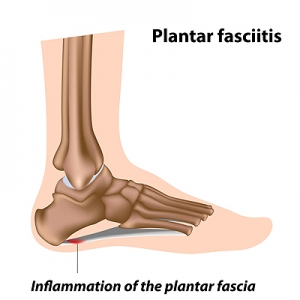
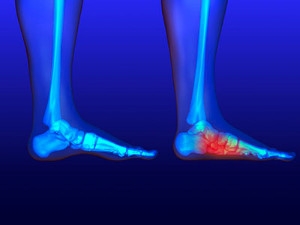
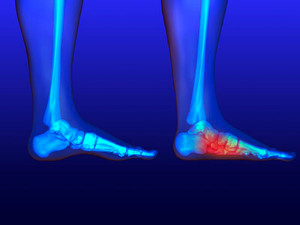
Plantar fasci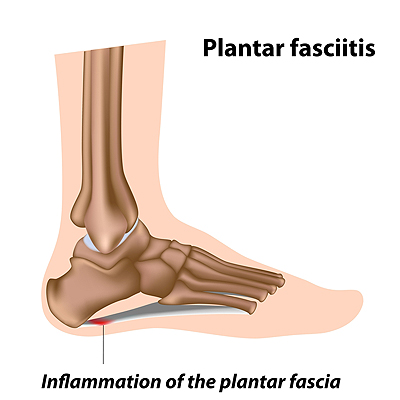 itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
itis is the inflammation of the plantar fascia, which is the band of tissue that runs along the bottom of the foot from the heel to the toes. A common sign of plantar fasciitis is pain in the heel as well as the arch of the foot. The pain is usually worse when taking your first few steps right after sleeping or resting, and it may ease during exercise and worsen afterwards. Common risk factors for plantar fasciitis include exercising with a tight calf, recently starting to exercise on hard surfaces, wearing shoes with poor support, and being overweight. Patients who have heel pain that is stopping them from doing daily activities, that keeps getting worse, has not improved, or who also have diabetes should consult with a podiatrist for a proper diagnosis and treatment for the pain.
Plantar fasciitis can be very painful and inconvenient. If you are experiencing heel pain or symptoms of plantar fasciitis, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is Plantar Fasciitis?
Plantar fasciitis is the inflammation of the thick band of tissue that runs along the bottom of your foot, known as the plantar fascia, and causes mild to severe heel pain.
What Causes Plantar Fasciitis?
- Excessive running
- Non-supportive shoes
- Overpronation
- Repeated stretching and tearing of the plantar fascia
How Can It Be Treated?
- Conservative measures – anti-inflammatories, ice packs, stretching exercises, physical therapy, orthotic devices
- Shockwave therapy – sound waves are sent to the affected area to facilitate healing and are usually used for chronic cases of plantar fasciitis
- Surgery – usually only used as a last resort when all else fails. The plantar fascia can be surgically detached from the heel
While very treatable, plantar fasciitis is definitely not something that should be ignored. Especially in severe cases, speaking to your doctor right away is highly recommended to avoid complications and severe heel pain. Your podiatrist can work with you to provide the appropriate treatment options tailored to your condition.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot and ankle needs.
Plantar Fasciitis
The plantar fascia is a connective tissue in the heel that stretches across the bottom length of your foot. Plantar fasciitis occurs when the connective tissue becomes inflamed, causing heel pain and discomfort during physical activity. Although the condition is completely treatable, traditional methods can take up to a year to start becoming effective.
Plantar fasciitis is caused by a number of everyday activities, so understanding the condition is important for managing and treating it. One of the most common causes of plantar fasciitis is excessive running, especially with improper fitting or non-supportive shoes. Too much exercise can lead to the plantar fascia being overworked and overstretched, which can cause tears in the tissue. Along with improper fitting shoes, pronation, the rolling of the feet inward, is a common cause of plantar fasciitis. If not treated properly, the plantar fascia becomes overstretched and starts to tear, causing inflammation.
Despite the common causes of plantar fasciitis, there are many different treatment options. For less severe cases, conservative home remedies include taking anti-inflammatory drugs to alleviate pain, applying ice packs to the bottom of your foot and heel, slowly stretching and exercising your feet to re-strengthen the tissue, and using orthotic devices are all ways to help manage your plantar fasciitis.
For more severe cases, shockwave therapy has become a common solution for plantar fasciitis. Shockwave therapy can effectively break up the tissue on the bottom of your foot which facilitates healing and regeneration. This fights the chronic pain caused by plantar fasciitis. Even if this doesn’t work, surgery is always a final option. Surgery on the tissue itself can be done to permanently correct the issue and stop the inflammation and pain in your heels.
No matter what the case may be, consulting your podiatrist is the first and best step to recovery. Even the slightest amount of heel pain could be the first stage of plantar fasciitis. Untreated symptoms can lead to the tearing and overstretching of tissue. Because the tearing of tissue can be compounded if it remains ignored, it can evolve into a severe case. The solution is early detection and early treatment. Talk to your podiatrist about the possibilities of plantar fasciitis if you’re experiencing heel pain.
Fungi That Cause Toenail Infections
 Fungi are microorganisms that get their nutrients from a host. There are various kinds of fungi—some of which can cause infections (mycosis). Fungal infections can be spread either through person-to-person contact or exposure to contaminated surfaces. Onychomycosis is a fungus that affects the nails and nail beds—most commonly on the toes. If you have toenail fungus you may notice discoloration or scaling that appears under the nail, your nail may flake or crumble, or even separate from the nail bed. Over time, the nail can thicken and become brittle. If you do have a fungal infection, it may take months, even years to go away—if it all. A podiatrist can test your nail to make a proper diagnosis and treat toenail fungus properly through a variety of treatments including prescription medications, nail debridement, or laser therapy.
Fungi are microorganisms that get their nutrients from a host. There are various kinds of fungi—some of which can cause infections (mycosis). Fungal infections can be spread either through person-to-person contact or exposure to contaminated surfaces. Onychomycosis is a fungus that affects the nails and nail beds—most commonly on the toes. If you have toenail fungus you may notice discoloration or scaling that appears under the nail, your nail may flake or crumble, or even separate from the nail bed. Over time, the nail can thicken and become brittle. If you do have a fungal infection, it may take months, even years to go away—if it all. A podiatrist can test your nail to make a proper diagnosis and treat toenail fungus properly through a variety of treatments including prescription medications, nail debridement, or laser therapy.
For more information about treatment, contact one of our podiatrists of Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Toenail Fungus Treatment
Toenail fungus is a condition that affects many people and can be especially hard to get rid of. Fortunately, there are several methods to go about treating and avoiding it.
Antifungals & Deterrence
Oral antifungal medicine has been shown to be effective in many cases. It is important to consult with a podiatrist to determine the proper regiment for you, or potentially explore other options.
Applying foot powder on the feet and shoes helps keep the feet free of moisture and sweat.
Sandals or open toed shoes – Wearing these will allow air movement and help keep feet dry. They also expose your feet to light, which fungus cannot tolerate. Socks with moisture wicking material also help as well.
If you have any questions please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic tools and technology to treat your foot and ankle needs.
How to Treat Your Toenail Fungus
While not a serious issue, toenail fungus, or onychomycosis, can be an embarrassing and uncomfortable condition to experience. Toenail fungus is often caused from public areas that harbor fungi and improper cleaning/drying of the foot. Once infected, the fungus grows deeper into the nail and can be very hard to get rid of.
There are different types of fungus that cause toenail fungus. Dermatophytes, yeasts, and molds are the most frequent forms of fungus to infect the toenail. Dermatophytes are the most common among the three. Symptoms associated with fungal nails include the discoloration of the toenail, brittleness, and in some circumstances, a smell. Pain is rarely a symptom caused by toenail fungus.
Diagnosis of fungal nails is generally a rather quick process. However podiatrists will make sure that the cause is not another condition such as lichen planus, psoriasis, onychogryphosis, or nail damage. Podiatrists will make use of fungal cultures and microscopy to verify that it is fungus.
While over-the-counter ointments are readily available, most are ineffective. This is due to the fact that the nail is very protective and that the fungus slips in between the nail plate and bed. Podiatrists can offer oral medication which currently provides the best results.
Ultimately, prevention is the best line of defense against toenail fungus. Avoid unsanitary public showers. If you do use a public shower, use shower shoes to provide your foot with protection. Once you are finished showering, make sure to thoroughly dry your feet. Fungi thrive in warm, dark, and moist places like sweaty, warm feet that are left dark in shoes all day.
An Association Between Obesity and Flat Feet
Being obese can put excess strain on your feet, so perhaps it is not surprising that there appears to be an association between being obese and having flatter feet. The term “flat foot” refers to a foot structure in which the arch that is normally present in the center of the bottom of the foot is not visible when the foot is bearing weight. Infants are born with flat feet, but most will develop an arch over time. Those who don’t will go on to have flat feet, but will usually not have any symptoms. Flat feet can also be acquired later in life as excess pressure on the feet, or the loosening of the plantar fascia ligament, causes the arch to collapse. Acquired flat foot may cause pain and discomfort in those who have it, and this issue appears to be more common in people who are obese, although whether or not there is a causative relationship remains uncertain. If you have any foot pain, please consult with a podiatrist.
The more you weigh, the harder your feet must work to support your body. If you’re an obese individual and are concerned about your feet, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Obesity and Your Feet
People who are overweight are putting more pressure on their ankles, knees, and hips as well as their feet. This unfortunately can lead to variety of different issues.
Problems & Complications Stemming from Obesity
- When the body is overweight, it tries to compensate by changing the way that it moves. An obese person may lean forward and put extra weight on the wrong part of the foot. This puts unnecessary stress on the feet.
- Obese people are also more likely to develop type II diabetes which is a condition that causes a lot of foot problems. People with diabetes often don’t feel the cuts and sores that they may have on their feet, which can lead to more complicated and severe issues.
- Plantar fasciitis is another foot condition that can be caused by obesity. Plantar fasciitis is an inflammation of the tissue along the bottom of the foot, which causes pain and stiffness while walking and climbing stairs.
If you have any questions, please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
Obesity and the Feet
Obesity is a common problem in American society. Approximately one third of the U.S. population is obese. Obesity is defined as a body mass index greater than 30. Obesity has the power to affect different aspects of the body, and one of the most common problems it causes is foot pain. There have been many studies that found a connection between an increased BMI and foot problems. A simple activity such as walking up a flight of stairs can increase pressure on the ankle by four to six times.
Being overweight causes the body to compensate for the extra weight by changing the way it moves. Consequently, people who struggle with obesity commonly have arch problems in their feet. Obesity causes the arch to break by stretching the ligaments and tendons that hold the bones in the foot together. When the arch lowers, the foot may eventually fall flat. Collapsed foot arches fail to provide adequate shock absorption which eventually leads to foot pain. Other conditions that may be caused by flat feet are pronation, plantar fasciitis, weak ankles, and shin splints.
Foot problems that are caused by obesity may be treated by wearing proper footwear. Proper shoes will allow your feet to have better circulation around the arch and ankle. Additionally, those with obesity often discover that typical heel pain remedies are not effective for them. They will find that their plantar fascia is easily injured, and it is often inflamed. The best way to treat this problem is to implement lifestyle changes. A few good ways to improve your diet are to reduce calories, fill up on fruits and veggies, and to limit sugars.
Custom foot orthotics can prevent foot problems if you’re carrying excess weight or are trying to lose weight. The purpose of orthotics is to provide shock absorption to decrease the amount of stress on the joints to prevent arthritis.
Bunions 101
 Bunions are a very common foot condition that develops at the main joint of the big toe and appears as a bony lump. Bunions are formed when the joint in the big toe gets pulled out of alignment and is turned towards the rest of the toes. Bunions can be formed due to a variety of factors that include a poor mechanical structure from genetics, footwear that fits poorly and is too narrow, age, or arthritis. Bunions can be painful and can interfere with wearing everyday footwear. Most treatments for bunions focus on relieving the pain caused by them, since surgery is the only option for correcting a bunion. Conservative or nonsurgical treatment options that a podiatrist may recommend include exercises, night splints, and shoe inserts. If you are struggling with a painful bunion, consulting with a podiatrist is suggested. A podiatrist will help you find a proper treatment method for managing the bunion and help determine if surgery is right for you.
Bunions are a very common foot condition that develops at the main joint of the big toe and appears as a bony lump. Bunions are formed when the joint in the big toe gets pulled out of alignment and is turned towards the rest of the toes. Bunions can be formed due to a variety of factors that include a poor mechanical structure from genetics, footwear that fits poorly and is too narrow, age, or arthritis. Bunions can be painful and can interfere with wearing everyday footwear. Most treatments for bunions focus on relieving the pain caused by them, since surgery is the only option for correcting a bunion. Conservative or nonsurgical treatment options that a podiatrist may recommend include exercises, night splints, and shoe inserts. If you are struggling with a painful bunion, consulting with a podiatrist is suggested. A podiatrist will help you find a proper treatment method for managing the bunion and help determine if surgery is right for you.
If you are suffering from bunion pain, contact one of our podiatrists of Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
What Is a Bunion?
Bunions are painful bony bumps that usually develop on the inside of the foot at the joint of the big toe. As the deformity increases over time, it may become painful to walk and wear shoes. Women are more likely to exacerbate existing bunions since they often wear tight, narrow shoes that shift their toes together. Bunion pain can be relieved by wearing wider shoes with enough room for the toes.
Causes
- Genetics – some people inherit feet that are more prone to bunion development
- Inflammatory Conditions - rheumatoid arthritis and polio may cause bunion development
Symptoms
- Redness and inflammation
- Pain and tenderness
- Callus or corns on the bump
- Restricted motion in the big toe
In order to diagnose your bunion, your podiatrist may ask about your medical history, symptoms, and general health. Your doctor might also order an x-ray to take a closer look at your feet. Nonsurgical treatment options include orthotics, padding, icing, changes in footwear, and medication. If nonsurgical treatments don’t alleviate your bunion pain, surgery may be necessary.
If you have any questions, please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.
What Are Bunions?
Bunions are large bony bumps at the base of the big toe. Medically known as hallux valgus, a bunion is a misalignment of the metatarsophalangeal joint, or big toe joint. The misalignment will generally worsen with time if left untreated.
The exact cause of bunions is unknown, with genetics seen as a potential cause. High heels and poorly-fitted footwear, rheumatoid arthritis, and heredity all seem to be potential factors behind the exacerbation of bunions. Women have been found to be more likely to develop bunions in comparison to men.
Bunions do not always produce symptoms. The best way to tell is if the big toe is pushing up against the next toe and there is a large protrusion at the base of the big toe. You may or may not feel pain. Redness, swelling, and restricted movement of the big toe may be present as well.
Podiatrists use a variety of methods to diagnose bunions. If there are symptoms present, podiatrists will first consider that it is a bunion. If not, a physical examination will be conducted to check function of the big toe. Finally, an X-ray may be taken to view the extent of the bunion and confirm it is a bunion.
Typically, nonsurgical methods are used to treat bunions, unless the bunion has become too misaligned. Orthotics, icing and resting the foot, roomier and better fitted shoes, taping the foot, and pain medication are usually utilized first. If the bunion doesn’t go away or causes extreme pain, surgery may be required. Surgeons will either remove part of the swollen tissue or bone to straighten the toe out.
If you have a bunion, it is recommended to see a podiatrist. The longer it is left untreated, the worse it may get. Podiatrists can properly diagnose and treat a bunion before it gets worse.
Why Are My Heels Cracked?
 Dry, cracked heels can be not only annoying and unsightly, but also painful. The biggest cause of cracked heels is skin dehydration. The skin on the bottom of the feet tends to lose moisture easily. This can occur from a variety of factors, such as exposure to dry indoor heating, cold weather and from wearing shoes that do not protect the back of the foot. Once the feet become dehydrated, the skin can become rough and thick, forming calluses to protect the heel. Over time, the calluses can crack, and can cause discomfort, pain, and even infection. If you notice that your heels are dry, cracked, itchy, tender, or discolored, it is suggested that you seek the care of a podiatrist.
Dry, cracked heels can be not only annoying and unsightly, but also painful. The biggest cause of cracked heels is skin dehydration. The skin on the bottom of the feet tends to lose moisture easily. This can occur from a variety of factors, such as exposure to dry indoor heating, cold weather and from wearing shoes that do not protect the back of the foot. Once the feet become dehydrated, the skin can become rough and thick, forming calluses to protect the heel. Over time, the calluses can crack, and can cause discomfort, pain, and even infection. If you notice that your heels are dry, cracked, itchy, tender, or discolored, it is suggested that you seek the care of a podiatrist.
Cracked heels are unsightly and can cause further damage to your shoes and feet. If you have any concerns, contact one of our podiatrists from Princeton Foot and Ankle Associates. Our doctors can provide the care you need to keep you pain-free and on your feet.
Cracked Heels
Cracked heels appear unappealing and can make it harder for you walk around in sandals. Aside from looking unpleasant, cracked heels can also tear stockings, socks, and wear out your shoes. There are several methods to help restore a cracked heel and prevent further damage.
How Do You Get Them?
Dry skin is the number one culprit in creating cracked heels. Many athletes, walkers, joggers, and even swimmers suffer from cracked heels. Age and skin oil production play a role to getting cracked heels as well.
Promote Healing
Over the counter medicines can help, especially for those that need instant relief or who suffer from chronic dry feet.
Wear Socks – Wearing socks with medicated creams helps lock in moisture.
Moisturizers – Applying both day and night will help alleviate dryness which causes cracking.
Pumice Stones – These exfoliate and remove dead skin, which allows for smoother moisturizer application and better absorption into the skin.
Change in Diet
Eating healthy with a well-balanced diet will give the skin a fresh and radiant look. Your body responds to the kinds of food you ingest. Omega-3 fatty acids and zinc supplements can also revitalize skin tissue.
Most importantly, seek professional help if unsure how to proceed in treating cracked heels. A podiatrist will help you with any questions or information needed.
If you have any questions, please feel free to contact our offices located in Princeton, and West Windsor, NJ . We offer the newest diagnostic and treatment technologies for all your foot care needs.